Venturing into new possibilities
Venturing into new possibilities Mines has long been renowned for being innovative in the...
Apr 25, 2024
Venturing into new possibilities Mines has long been renowned for being innovative in the...



Apr 7, 2023

Jan 12, 2023

Nov 8, 2022
Apr 25, 2024
The best job in the world Some have said that being a university president is the toughest or even...

Apr 25, 2024

Jan 23, 2024

Jan 23, 2024

Jan 23, 2024

Apr 25, 2024
Supporting new ventures Zack Bennett ’99 has always been an explorer, curious about the unknown...

Apr 25, 2024

Apr 25, 2024

Apr 25, 2024

Jan 23, 2024

Jan 23, 2024
Apr 25, 2024
Supporting new ventures Zack Bennett ’99 has always been an explorer, curious about the unknown...

Apr 25, 2024

Jan 23, 2024

Jan 23, 2024
Apr 25, 2024
Combining scientific expertise Mines and the U.S. Geological Survey established a joint industry...

Apr 25, 2024
Apr 25, 2024
Apr 25, 2024
Apr 25, 2024
Engineering campus When Conor Lenon ’14, MS ’15 was a Mines student, he remembers that the Mines...

Apr 25, 2024

Jan 23, 2024

Jan 23, 2024
The best job in the world Some have said that being a university president is the toughest or even...
Read MoreSweeping success For the first time in program history, Mines’ men’s and women’s track & field...
Read MoreIn full swing In 1980, the average driving distance of professional golfers on the PGA Tour was...
Read MoreCombining scientific expertise Mines and the U.S. Geological Survey established a joint industry...
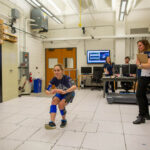
Read MoreMoving the needle for movement sciences There’s still a lot to learn in the field of movement...
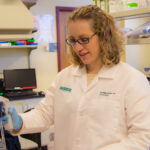
Read MoreBetter care for wound healing Colorado-based biomaterials company GelSana Therapeutics has...
Read MoreSupporting new ventures Zack Bennett ’99 has always been an explorer, curious about the unknown...
Read MoreBuilding on traditions, connections and impact The M Climb. Oredigger Camp. Senior Capstone Design...
Read MoreCreating a sense of communal support The theme of this year’s Forces of Mines: Elevating Women...
Read MoreAll in the family As current Mines student Rowan Welch makes his way around the Mines campus, he...
Read MoreLeading with integrity Chris Valdez ’00 and Ty Harrison ’98 first met as Mines students and both...
Read MoreEngineering campus When Conor Lenon ’14, MS ’15 was a Mines student, he remembers that the Mines...
Read MoreVenturing into new possibilities Mines has long been renowned for being innovative in the...
Read More
